

Medical stock photos of people in the medical industry i.e. nurses, clinicians, doctors, hospital staff, and the patients they serve.



Because the symptoms of influenza can be similar to those caused by other infectious agents, the disease can be difficult to diagnose based on clinical symptoms alone. A number of tests can help in the diagnosis of influenza, but testing does not need to be done for all patients. During an outbreak of respiratory illness, testing for influenza can help determine if influenza is the cause of the outbreak.
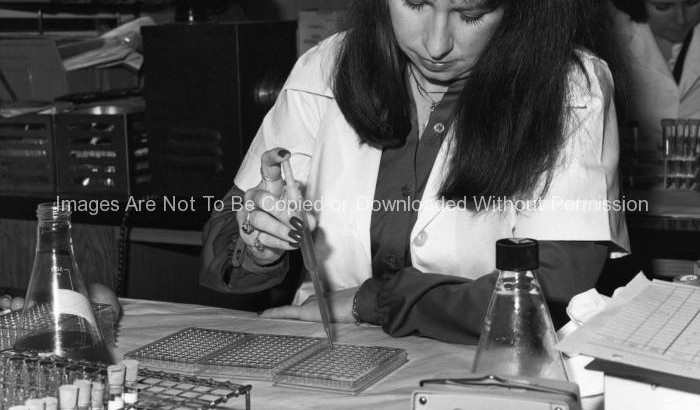
The presence or absence of influenza virus would be determined by using an agglutination test. If it involved the agglutination, or clumping of red blood cells (RBCs), the phenomenon is known as hemoagglutination.
Diagnostic tests available for influenza include viral culture, serology, rapid antigen testing, polymerase chain reaction (PCR), and immunofluorescence assays. Sensitivity and specificity of any test for influenza might vary by the laboratory that performs the test, the type of test used, and the type of specimen tested. Among respiratory specimens for viral isolation or rapid detection, nasopharyngeal specimens are typically more effective than throat swab specimens. As with any diagnostic test, results should be evaluated in the context of other clinical and epidemiologic information available to health-care providers.

This photograph depicts post-doctoral fellow, Neal Van Hoeven, Ph.D. as he was demonstrating how one is to properly wear personal protective equipment (PPE), in appropriate laboratory settings. PPE includes Dr. Hoeven’s gloves, surgical gown, and his N95 respirator.
Personal protective equipment, or PPE, as defined by the Occupational Safety and Health Administration, or OSHA, is “specialized clothing or equipment, worn by an employee for protection against infectious materials.”
OSHA issues regulations for workplace health and safety. These regulations require use of PPE in healthcare settings to protect healthcare personnel from exposure to bloodborne pathogens and Mycobacterium tuberculosis. However, under OSHA’s General Duty Clause PPE is required for any potential infectious disease exposure. Employers must provide their employees with appropriate PPE and ensure that PPE is disposed or, if reusable, that it is properly cleaned or laundered, repaired and stored after use.
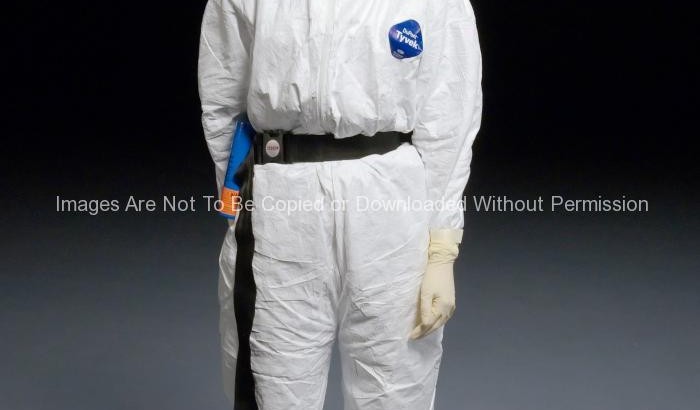
This photograph depicts post-doctoral fellow, Jessica Belser, Ph.D. as she was demonstrating how one is to properly wear personal protective equipment (PPE), in appropriate laboratory settings. PPE includes Dr. Belser’s Tyvek® suit, double gloves, and her powered air purifying respirator.
Personal protective equipment, or PPE, as defined by the Occupational Safety and Health Administration, or OSHA, is “specialized clothing or equipment, worn by an employee for protection against infectious materials.”
OSHA issues regulations for workplace health and safety. These regulations require use of PPE in healthcare settings to protect healthcare personnel from exposure to bloodborne pathogens and Mycobacterium tuberculosis. However, under OSHA’s General Duty Clause PPE is required for any potential infectious disease exposure. Employers must provide their employees with appropriate PPE and ensure that PPE is disposed or, if reusable, that it is properly cleaned or laundered, repaired and stored after use.
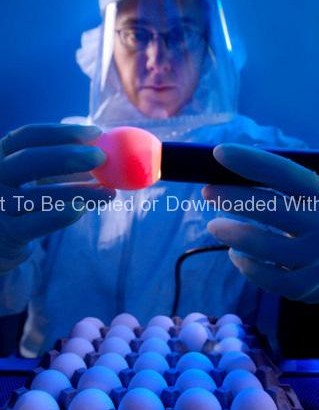
This 2008 photograph depicted CDC microbiologist, Amanda Balish, as she was demonstrating how one properly “candles” an embyonated chicken egg, which employs a very bright light that is either placed behind the egg, such as was done throughout history by using a candle, hence the name, or employing more modern methods, using a powerful lamp placed against the broad end of the egg, as was the case here. In this way, the contents of the egg are revealed through the translucent shell. By using this procedure, Amanda was able to access the viability of each egg used in the isolation of influenza viruses.
If the egg is unfertilized the observer will see only a round yolk sac, and no developing embryo, or any network of blood vessels. Unfertilized eggs are known as “yolkers”. Eggs known as “quitters”, had been fertilized, but the embryo had stopped growing. In the case of quitters, one will note a thin blood ring encircling the yolk, as seen in PHIL 10148. “Winners” are eggs that had been fertilized, and lead to the growth of a healthy embryo, which is seen in PHIL 10149. In this case, one will observe numbers of networked blood vessels surrounding the yolk, and depending upon the length of gestation, one might see a dark shadow representing the developing embryonic eye.

Arnold Steigerwalt, a research chemist with the Centers for Disease Control’s Meningitis and Special Pathogens Branch (MSPB) in the National Center for Infectious Diseases (NCID), was shown here as he was performing a DNA-DNA hybridization analysis in one of the CDC’s laboratories.
The Meningitis and Special Pathogens Branch is responsible for monitoring an eclectic group of bacterial infections and disease syndromes of public health importance. The branch is organized into programs on meningitis, which focuses on Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae, vaccine-preventable diseases of childhood, which deals with Bordetella pertussis and Corynebacterium diphtheriae, zoonotic pathogens, which works with Bacillus anthracis, Brucella spp., Leptospires, and “non-tuberculosis” mycobacterial infections, and unexplained deaths and other emerging infections.

Sandra Bragg, Ph.D., of the Centers for Disease Control’s Meningitis and Special Pathogens Branch (MSPB) in the National Center for Infectious Diseases (NCID), was shown seated in front of a microscope, as she was reading a Microscopic Agglutination Test (MAT) by using dark field microscopy.
The Meningitis and Special Pathogens Branch is responsible for monitoring an eclectic group of bacterial infections and disease syndromes of public health importance. The branch is organized into programs on meningitis, which focuses on Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae, vaccine-preventable diseases of childhood, which deals with Bordetella pertussis and Corynebacterium diphtheriae, zoonotic pathogens, which works with Bacillus anthracis, Brucella spp., Leptospires, and “non-tuberculosis” mycobacterial infections, and unexplained deaths and other emerging infections.

Renee Galloway, a microbiologist in the Centers for Disease Control’s Meningitis and Special Pathogens Branch (MSPB), in the National Center for Infectious Diseases (NCID), was shown here running a Pulsed-field Gel Electrophoresis (PFGE) analytical test, which is used in the typing of bacterial organisms.
The Meningitis and Special Pathogens Branch is responsible for monitoring an eclectic group of bacterial infections and disease syndromes of public health importance. The branch is organized into programs on meningitis, which focuses on Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae, vaccine-preventable diseases of childhood, which deals with Bordetella pertussis and Corynebacterium diphtheriae, zoonotic pathogens, which works with Bacillus anthracis, Brucella spp., Leptospires, and “non-tuberculosis” mycobacterial infections, and unexplained deaths and other emerging infections.

This 2005 photograph of the Centers for Disease Control and Prevention’s Dr. Terrence Tumpey, one of the organization’s staff microbiologists and a member of the National Center for Infectious Diseases (NCID), showed him examining reconstructed 1918 Pandemic Influenza Virus inside a specimen vial containing an orange-colored supernatant culture medium.
Dr. Tumpey, here seen in a Biosafety Level 3-enhanced laboratory setting, was working beneath a flow hood, which pulls air from outside the hood into the hood’s confines, and is then filtered of any pathogens before being re-circulated inside the self contained laboratory atmosphere.
Dr. Tumpey recreated the 1918 influenza virus in order to identify the characteristics that made this organism such a deadly pathogen. Research efforts such as this, enables researchers to develop new vaccines and treatments for future pandemic influenza viruses.
The 1918 Spanish flu epidemic was caused by an influenza A (H1N1) virus, killing more than 500,000 people in the United States, and up to 50 million worldwide. The possible source was a newly emerged virus from a swine or an avian host of a mutated H1N1 virus. Many people died within the first few days after infection, and others died of complications later. Nearly half of those who died were young, healthy adults. Influenza A (H1N1) viruses still circulate today after being introduced again into the human population in the 1970s.